Hepatitis C is a type of viral hepatitis that is transmitted through blood and eventually causes liver disease in most patients. Approximately 130-150 million people across the nation have the hepatitis C virus (HCV).[1] For them, this means a lifetime of potentially uncomfortable symptoms and serious risks to their health. In severe cases, sufferers may ever experience liver failure and death. Managing these symptoms can be difficult, and the virus is best handled when caught early. That being said, receiving an HCV diagnosis doesn’t mean you’re doomed to a life of pain and disability. In fact, most people that adequately treat their HCV go on to live healthy lives.
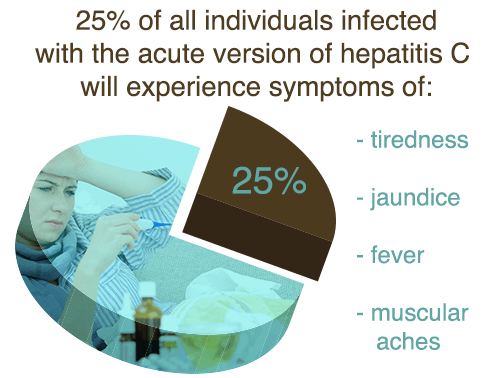
The virus poses serious threats when left untreated, which is common for many because it is often asymptomatic in nature. Around 25 percent of all individuals infected with the acute version of hepatitis C will experience symptoms of tiredness, jaundice, fever, and muscular aches and pains.[2] The chronic version of the virus generally presents more symptoms as it begins to attack the liver and inflame it. Elevated liver enzymes often point to the possibility of the hepatitis C virus in blood tests. In 2001, about 2.7 million people were chronically infected with hepatitis C in America, and 25,000 of them were new cases.[3]
Hepatitis C can segue back and forth from active to dormant. When inactive, the infected party won’t present any symptoms, but there is no concrete evidence to support the much-touted theory that the virus is no longer contagious in these stages — even in cases where the virus has been dormant for many years.
Who Gets HCV?
When it comes to hepatitis C, injection drug users (IDU) are most affected. It is estimated that around 1 million people in the United States are IDUs.[4] Many IDUs will engage in substance abuse practices with peers without using sterile equipment, and some even share needles. This makes the passage of the virus from an infected individual to an uninfected person highly likely. Within the first six months to a year of injecting drugs, 50-80 percent of IV drug users will contract HCV.[5]
Even if you don’t inject drugs, being a substance abuser still puts you at a higher risk of contracting an infectious disease like HCV. Likewise, there are other diseases to worry about, too, such as HIV. Among IDUs, 50-90 percent of those who are infected with HIV due to their injection drug use also have HCV.[6] Those who snort drugs like cocaine are also at risk if they’re sharing equipment with someone else. While the risk is much lower in sexual partners who engage in frequent intimate contact, it’s still there at a 1 percent transmission rate.[7] Others who are at risk for contracting HCV include:
- Children born to HCV-positive mothers
- Individuals with body piercings or tattoos
- People with multiple, high-risk sex partners
- Individuals on dialysis
- People who received blood transfusions prior to 1990[8]
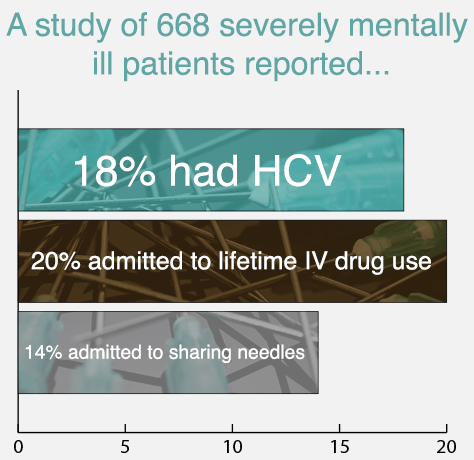
Surprisingly, those with mental illness are also more likely to have hepatitis C, mostly due to their conjunctive elevated risk of substance abuse. Around half of all individuals diagnosed with a severe mental health disorder are also engaging in drug or alcohol abuse.[9] In one study of 293 HCV patients, 93 percent had at least one psychiatric disorder in the present or past, and 73 percent had two or more.[10] Another study of 668 severely mentally ill patients reported 18 percent had HCV, and over 20 percent of the sample admitted to lifetime IV drug use and 14 percent to sharing needles.[11] In addition, 57 percent reported that they had sniffed or snorted cocaine, and 39 percent had smoked crack.[12]
Alcohol abuse isn’t going put you on a path to contracting HCV all on its own, but if you have the disease, booze will make matters worse. Since alcohol abuse is more common in drug abusers, it stands to reason that IDUs with HCV may be at risk for additional liver damage, caused by adding alcohol to the mix. The results of one study show that the risk of cirrhosis is increased threefold in people who drink heavily for at least a decade, whether they have HCV or not.[13] Elaborating on that, among those who do have HCV, 32 percent who drank heavily had cirrhosis whereas only 10 percent of those who didn’t drink heavily had it.[14] Additional research confirms that fibrosis and liver scarring are more common in HCV-infected patients who drink more than average amounts of alcohol.[15]
Life With Hepatitis C
While it is certainly scary to wait for the test results for any illness, HCV can seem like a life sentence. Don’t be discouraged. Early diagnosis means better treatment and a shot at clearing the infection altogether. This means you’re on the right path to a long and healthy life that awaits you. Living with hepatitis C is no longer viewed as the curse it once was. In fact, recent research points to a potential cure for the virus, noting success rates nearing 90 percent in one study using a combination of sofosbuvir and simeprevir.[16]
Around 20 percent of all people who are exposed to the virus will naturally fight it off and clear it from their system.[17] The idea of curing HCV is surely a hot topic of debate among medical professions, with many still touting its impossibility. HCV progresses in only about 50-60 percent of cases.[18] Among them, current mainstream antiviral medication therapies are successful in reducing symptoms and virus levels in around 50-75 percent of patients.[19] Despite the success of readily available treatment, less than 40 percent of HCV-infected individuals seek treatment for their condition, and only 5 to 6 percent receive antiviral treatment.[20]
HCV is not deadly in and of itself, but the issues that come from it often are. Liver disease is the biggest issue that stems from the virus, and 70 percent of those who are chronically infected will end up with it.[21] Among them, 15 percent will develop cirrhosis.[22] The average patient who is otherwise in good health can expect to live many decades with the virus. That being said, it can indeed shorten one’s lifespan. In one study of 11,703 people with HCV, 14 percent died during the study, 60 percent were between the ages of 45 and 59, and 34 percent were 60 and up.[23] Compared to another study in which patients died from multiple causes of death, those with the HCV died 15 years earlier and their mortality rate was 12 times higher.[24] Every year, between 8,000 and 10,000 people die from health ailments stemming from HCV.[25]
Simultaneous Treatment Approach
A quality rehabilitation facility can treat both HCV and substance abuse issues at the same time. First and foremost, HCV and any other underlying or previously diagnosed health problems must be brought to a manageable state before moving forward with a full course of drug therapy. This is of high importance for anyone who plans to enter treatment where medication may be required, such as opiate abusers in seek of a medicated maintenance program. It is necessary that the individual is stable and in good enough health to tolerate prescription medications and withdrawal. In most cases, this isn’t an issue, and the majority of patients find that the symptoms of HCV begin to decrease as their addiction wanes.
Furthermore, detox and treatment that is medically supervised are highly encouraged for the HCV-infected patient. Those with mental health problems stand to benefit even more. In either case, managing multiple medications during treatment isn’t advisable without a skilled physician overseeing the process every step of the way.
The traditional medical approach to treating HCV has been a combined therapy of pegylated interferon and ribavirin tablets over the course of 6-11 months — a treatment that cured up to half of its patients.[26] In the past few years, another treatment method has come to the surface and promises a nearly 70 percent success rate in new treatment patients.[27] Protease inhibitors shorten treatment time and are just the beginning of what is expected to develop in HCV medication treatment department in coming years.
Fortunately, new inventions in modern medical technology and the promotion of safe injection practices — and deterrence toward sharing needles — have lowered the rate of infectious disease across the board in America over the years. In addition, donated organs and blood weren’t screened for HCV in the US until 1992; today, that is no longer an issue.[28]
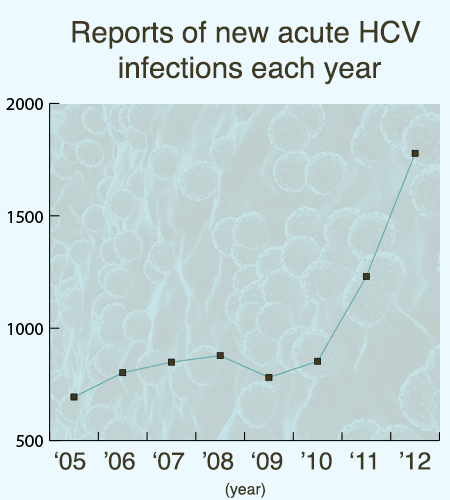
Between 1989 and 2005, the rate of new HCV infections in this country fell by 90 percent.[29] However, since then, the rate of new infections is actually rising steadily. Reports of new acute HCV infections were at 694 in 2005, 802 a year later, 849 in 2007, and 878 in 2008. They then dipped to 781 in 2009.[30] This recession wouldn’t last though, as the rate spiked to 853 in 2010, 1,230 in 2011, and then 1,778 in 2012.[31] Since these are reported new cases, the actual number of cases is expected to be substantially higher. Nationwide, as many as 3.9 million cases of chronic HCV are suspected.[32]
The number of deaths from the virus continues to rise, mostly due to poor screening practices. With injection drug users making up the majority of the HCV-infected population, it isn’t surprising that many — if not most — of those who are infected don’t have health insurance and don’t see a doctor for an annual physical. In fact, 59.6 percent of individuals aged 26 and older who sought substance abuse treatment in 2011 reported not having any health insurance.[33] It’s expected that the number of deaths from hepatitis C will continue to rise over the coming years. Predictions are based on knowledge that the majority of HCV infections are still coming to light and may take 20-30 years to run their course.
Hepatitis C is not a death sentence, but proper care is essential. If one is suffering from both HCV and addiction, it’s essential to seek comprehensive treated as soon as possible. In 2013, 43,982 people died from drug-related overdoses in America.[34] With proper care, both issues can be managed, helping to ensure better health and a longer life.
Citations
[1] “Hepatitis C.” (2014 April). World Health Organization. Accessed March 19, 2015.
[2] Nettleman, M. (2014 February 2). “Hepatitis C.” MedicineNet. Accessed March 19, 2015.
[3] “Viral Hepatitis and Injection Drug Users.” (n.d.). National Alliance of State and Territorial AIDS Directors. Accessed March 19, 2015.
[4] Ibid.
[5] “Who Is At Risk for Hepatitis C?” (n.d.). WebMD. Accessed March 19, 2015.
[6] “Viral Hepatitis and Injection Drug Users.” (n.d.). National Alliance of State and Territorial AIDS Directors. Accessed March 19, 2015.
[7] “Who Is At Risk For Hepatitis C?” (n.d.). WebMD. Accessed March 19, 2015.
[8] Ibid.
[9] “Substance Abuse and Co-Occurring Disorders.” (n.d.). National Alliance on Mental Illness. Accessed March 19, 2015.
[10] Fireman, M., Indest, D.W., Blackwell, A., Whitehead, A.J. & Hauser, P. (2005 April 15). “Addressing tri-morbidity (hepatitis C, psychiatric disorders, and substance use): the importance of routine mental health screening as a component of a comanagement model of care.” Clinical Infectious Diseases. Accessed March 19, 2015.
[11] Osher, F.C., Goldberg, R.W., McNary, S.W., Swartz, M.S., Essock, S.M., Butterfield, M.I. & Rosenberg, S.D. (2003 June). “Substance abuse and the transmission of hepatitis C among persons with severe mental illness.” Psychiatric Services. Accessed March 19, 2015.
[12] Ibid.
[13] Schiff, E.R. & Ozden, N. (2004 September 29). “Hepatitis C and Alcohol.” National Institute on Alcohol Abuse and Alcoholism. Accessed March 19, 2015.
[14] Ibid.
[15] Ibid.
[16] Krans, B. (2013 November 13). “Life After Hepatitis C: It’s No Longer A ‘Death Sentence’.” Healthline News. Accessed March 19, 2015.
[17] Case-Lo, C. (2014 April 11). “Dangerous Cocktail: Alcohol and Hepatitis C.” Healthline. Accessed March 19, 2015.
[18] Lieber, C.S. (n.d.). “Alcohol and Hepatitis C.” National Institute on Alcohol Abuse and Alcoholism. Accessed March 19, 2015.
[19] Ibid.
[20] Acosta Scott, J. (2014 May 15). “The Dangers of Untreated Hepatitis C.” Everyday Health. Accessed March 19, 2015.
[21] “Viral Hepatitis and Injection Drug Users.” (n.d.). National Alliance of State and Territorial AIDS Directors. Accessed March 19, 2015.
[22] Ibid.
[23] “Hep C Takes 15 Years Off Life Span, Raises Death Risk 12-Fold.” (2013 October 21). Hepatitis Magazine. Accessed March 19, 2015.
[24] Ibid.
[25] Davies, P. (2005 May 31). “Long-Dormant Threat Surfaces: Deaths From Hepatitis C Are Expected to Triple” The Wall Street Journal. Accessed March 19, 2015.
[26] Norris, J. (2012 February 23). “Hepatitis C, a Leading Killer, Is Frequently Undiagnosed But Often Curable.” University of California San Francisco. Accessed March 19, 2015.
[27] Ibid.
[28] “How is Hepatitis C Transmitted or Spread?” (n.d.). American Liver Foundation. Accessed March 19, 2015.
[29] Davies, P. (2005 May 31). “Long-Dormant Threat Surfaces: Deaths From Hepatitis C Are Expected to Triple” The Wall Street Journal. Accessed March 19, 2015.
[30] “Viral Hepatitis Statistics and Surveillance.” (2008 June 24). Centers for Disease Control and Prevention. Accessed March 19, 2015.
[31] Ibid.
[32] Ibid.
[33] “Health Insurance Status of Adult Substance Abuse Treatment Admissions Aged 26 or Older: 2011.” (2014 February 6). Substance Abuse and Mental Health Services Administration. Accessed March 19, 2015.
[34] “Prescription Drug Overdose in the United States: Fact Sheet.” (2014 October 17). Centers for Disease Control and Prevention. Accessed March 19, 2015.


