People who can do two things at once are typically considered to be quite talented. Talking on the phone and typing, listening to the radio while working, and cooking dinner and listening to a chattering child are all examples of multitasking that would merit a person at least some recognition, if not out-and-out admiration.
Unfortunately, there are times when doing two things at once means facing serious problems. Those who foster an addiction while maintaining a mental illness, for example, might very well be juggling two competing sets of priorities at the same time, undergoing mental acrobatics on a daily basis in a way that might baffle outsiders. But these people might also need specialized care in order to heal, and they might resist the very solutions that could help them.
Finding the Answer
When a person has both a mental illness and an addiction issue, experts refer to the condition as a “dual diagnosis” or a “co-occurring disorder.” Sometimes, the situation comes about due to the misery that mental illnesses can cause. For people torn apart by nervousness or brought low by depression, drugs and alcohol can seem like remarkable tools that can make pain fade away. In time, however, the substances that once brought relief can make discomfort much more acute, as the substances can do further damage to the cells of the brain.
 A person with chronic depression, for example, might feel a surge of joy after a hit of an opiate drug. The drug causes a boost of production of chemical signals of joy, and those might be the very signals the person has been missing due to depression. The drugs do seem to help, but in time, the cells of the brain might not produce any signals of pleasure at all unless drugs are present, and the person might need to take higher and higher doses of drugs to bring about pleasure. Without drugs, the person feels much more depressed than the person felt before the depression kicked in. At this point, the two conditions are intertwined.
A person with chronic depression, for example, might feel a surge of joy after a hit of an opiate drug. The drug causes a boost of production of chemical signals of joy, and those might be the very signals the person has been missing due to depression. The drugs do seem to help, but in time, the cells of the brain might not produce any signals of pleasure at all unless drugs are present, and the person might need to take higher and higher doses of drugs to bring about pleasure. Without drugs, the person feels much more depressed than the person felt before the depression kicked in. At this point, the two conditions are intertwined.
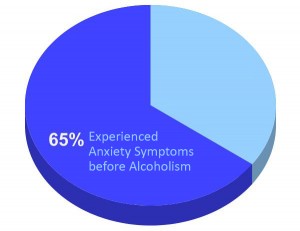
Research suggests that many people follow this kind of path toward a dual diagnosis. For example, a study in the Journal of Dual Diagnosis suggests that 65 percent of people who had both an alcoholism issue and an anxiety disorder experienced symptoms of anxiety well before the drinking began. Even so, some people do develop more persistent cases of mental illness only after they begin using drugs. Someone with an unstable personality who sometimes feels a little paranoid, for example, might transition into full-blown paranoiac hallucinations under the influence of drugs. It might be rare, but it certainly does happen.
Risk Associated With Drug Abuse
The National Institute of Mental Health conducted a study that looked at the increased risk factors for drug abuse when individuals suffered from other psychological disorders. They found that the condition with the highest increased risk to use and abuse drugs is associated with anti-social personality disorders. Those who suffer from personality disorders are nearly 15 percent more likely to abuse drugs or alcohol. Other conditions that increase risk of drug abuse are:
- Manic episodes (14.5 percent)
- Schizophrenia (10.1 percent)
- Panic disorders (4.3 percent)
- Major depressive episode (4.1 percent)
- Obsessive-compulsive disorders (3.4 percent)
- Various phobias (2.4 percent)
Treatment Decisions
In order for a dual diagnosis issue to be properly treated, experts must first diagnose the problem properly, and as an article in the Journal of Addictive Disorders makes clear, that can be difficult to do. In the early stages of recovery, it may be difficult for experts to find the source of behavioral difficulties, as some might be caused by mental illness and some might be caused by the withdrawal process. As a result, it’s not uncommon for experts to perform an in-depth assessment after detox, when the person is most likely to be sober. Any of these symptoms could be a sign of a mental illness, and when they appear in people who have admitted to a prior drug problem, they could indicate that a dual diagnosis issue is in play.
At this point, experts can attempt to identify:
- Gait changes or unusual movements
- Unusual beliefs
- Irrational thought patterns
- Erratic behaviors
- Hygiene issues
Finding Help
 Dual diagnosis issues are best treated in comprehensive programs that blend addiction care with mental health care. As the National Alliance on Mental Health puts it, “Effective integrated treatment consists of the same health professionals, working in one setting, providing appropriate treatment for both mental health and substance abuse in a coordinated fashion.” It’s a wraparound form of care that provides assistance for both problems at the same time.
Dual diagnosis issues are best treated in comprehensive programs that blend addiction care with mental health care. As the National Alliance on Mental Health puts it, “Effective integrated treatment consists of the same health professionals, working in one setting, providing appropriate treatment for both mental health and substance abuse in a coordinated fashion.” It’s a wraparound form of care that provides assistance for both problems at the same time.
Therapy plays a big role in a dual diagnosis program, and in each therapy session, clients are given the opportunity to think about how their mental health concerns and addiction concerns blend and intertwine. No one problem is given more importance than the other, and clients are encouraged to think of the complexities of managing their conditions in each therapy session they attend.
It’s not unusual, however, for people with dual diagnosis problems to need more than just therapy. Often, their lives have become so impaired due to their dysfunction that they need assistance in a variety of different areas. They might need housing assistance, legal assistance, employment training and more in order to pull together a life that’s free of severe difficulty, and they might need the help of many different types of caregivers, all working together, in order to bring about this kind of life overhaul. A trained mental health professional leads the team, of course, and ensures that all of the therapies provided have the ability to really transform a person’s life, but the care each member of the team provides can make a difference for a person with a dual diagnosis.
-
Common Treatment Methods
One of the most effective treatments for dual diagnosis patients has been the model of Cognitive Behavioral Therapy (CBT). This treatment program is a concise, regulated therapy that is based upon mutual communication, participation and trust between a provider and the patient. Rather than spending endless hours talking about and analyzing an individual, CBT is a 16-week program that includes self-assessments and homework assignments to teach the patient new ways to think (cognitive) and act (behavioral) without the use and abuse of drugs in their lives. The program takes place in both private sessions and groups, with role-playing activities and practical applications as important overall aspects. The program can be extended should the provider and the recovering addict decide more time is needed; however, when followed with adequate support, CBT has proven to be effective.
In addition to group and private therapy session, medications can be used to mitigate the effects of a dual diagnosis condition. Many of the psychological conditions that can lead to drug abuse, such as depression, anxiety or schizophrenia, can be managed with the proper diagnosis and medication. If the addict maintains their medications and uses them properly, it is possible that some of the feelings that originally drove them to abuse drugs can be assuaged. If these symptoms are no longer present, the likelihood that the addict will feel compelled to use drugs for the same reasons as in the past is greatly reduced.
-
Alternative Methods
Many treatment centers today offer myriad alternative therapies for addictions involving dual diagnosis. An alternative therapy is one that does not follow a traditional “provider-patient” model of treatment, but instead uses other sources to instill new thought patterns or treatments to an affected individual.
A few types of alternative therapy include:
- Animal Assisted Therapy: The use of horses to teach problem-solving skills and non-verbal communication skills.
- Reiki: For the discomfort and pain associated with withdrawal
- Meditation: To establish directions for otherwise unhealthy thought patterns
- Yoga: To help individuals regain dexterity and physical fitness after long-term drug use
- Martial Arts: For discipline of mind and body, as well as healthy conflict resolution and release of pent-up emotions
- Expressive Therapy: The effects of art and sound on the human mind have been well documented and can provide an outlet for emotions for the recovering addict
All of the above therapies develop the recovering addict’s abilities to problem-solve as well as their skill at avoiding interior and exterior conflicts in healthy and pragmatic ways. Many addicts suffering from dual diagnosis have a problem being alone due to the causes or effects of their underlying psychological condition. Some of these alternative therapies will help an individual learn that peaceful, quiet, alone time can be healing and provide solace from a troubled world.
When alternative therapies are used in conjunction with traditional treatments, the opportunities for success are greatly increased.
Make the Call
Living with a dual diagnosis can be difficult and stressful, and it’s not unusual for people with these concerns to feel as though no one can understand and help. If you’re feeling this way, we hope you’ll contact us at Axis.
We specialize in helping people just like you, and we have years of experience in both diagnosing a dual diagnosis problem and creating customized solutions that can bring real relief. All our counselors are adept at creating a safe and welcoming environment in which you can learn and grow, and we provide a significant amount of aftercare that can help you transition from our inpatient facility to your own neighborhood. With our help, you will be able to take control and you will find a sense of relief that’s been missing in the past. Please call us, and we’ll explain how the enrollment process works and how you can get started.







